Haringey Works is the council’s free employment and skills support service exclusively for the borough’s residents. There is no limit to the number of hours residents can spend with one of the advisors and there are no set ‘criteria’ to access and use the service other than being a Haringey resident looking for work.
In January 2019, Mrs E migrated from Greece to the UK with her husband and three children, to build a better life for her family. She visited Haringey Works office to receive support to find suitable employment. Due to English for Speakers of Other Languages (ESOL) barriers, initially the advisor had to use Google translator to communicate and was able to register Mrs E for employment support in the follow up appointments. Mrs E was supported with the National Recognition Information Centre (NARIC) to transfer qualifications to UK equivalent. Mrs E was supported with CV updates, interview skills and was also put forward via Haringey Works for a reablement worker role and was successful in securing this role. Since working with the advisor, she has completed the Entry 1 and 2 ESOL courses and is currently completing Entry 3.
Greater Manchester (GM) historically has a number of labour market inequalities, which have recently been exacerbated by COVID-19. The GM employment rate (75.5 per cent) is consistently below that of Great Britain (78.4 per cent) as a whole. Nearly a quarter of GM working age residents are economically inactive, compared to 21 per cent for England. GM has a working age population of 1.8M people, 221,000 of whom are claiming out of work benefits. As is well documented, there is a strong link between work and health, and 64 per cent of GM residents claiming out of work benefits have a health condition.
To combat this, Working Well, a system of integrated work, health and skills provision was created. Each of the Working Well programmes delivers to a different cohort of residents, from closest to furthest from the job market.
All programmes adhere to the same three delivery principles:
1.Personalised support
2. Local integration
3. An eco-system of work, health, and skills.
These principles were derived from a Test and Learn pilot from 2014 and are embedded into each Working Well contract.
Personalised Support
All Working Well programmes use a Key Worker model, meaning there is a single point of contact for each participant which allows relationships and trust to develop. The support of the programme is then tailored to the individual needs of the participant by making use of personalised action plans. The support is sequenced to ensure that the right support is delivered at the right time
Local Integration
Each programme integrates into each Greater Manchester borough and adapts to the local needs of the residents. Each Local Authority area has a designated Local Lead to liaise, support, and challenge delivery of these commissioned programmes. The programmes will also have designated members of staff who will build links with key stakeholders. Each locality will also develop an integration plan and will meet regularly at integration boards to ensure the programmes are embedded effectively.
Eco-System of Work, Health, and Skills
The broader system of support has been brought together to work towards a shared set of goals. The recently refreshed Greater Manchester Strategy outlines the goals and what needs to be done to impact them. Co-design and co-commissioning with key partners are also at the heart of this strategy and have been used on a number of Working Well programmes.
How to engage local partners to support the design of provision to meet local needs?
Locality-based Ask and Offer Documents
Each of the 10 Local Authorities of GM were consulted and an Ask and Offer document was created for each borough with respect to the local delivery of a specific programme. The document outlines what support the local authority can offer the provider by way of links to local organisations and businesses, additional resources etc. and makes requests of the provider such as sharing local data and taking part in regular local meetings.
These documents are developed during procurement to allow the information to shape local practices, governance and areas of focus. The documents can be referred to during live delivery to ensure that the local delivery intent is achieved. The documents are ‘live’ and adapt to continuous local need and management through local integration boards.
Co-commissioning
Programmes such as Working Well Early Help (WWEH), and Specialist Employment Service have been co-commissioned with partner organisations. In the case of WWEH, the programme was co-commissioned and co-funded by Greater Manchester Combined Authority, GM Health & Social Care Partnership and the Work and Health Unit. This process shaped the design and outcomes of the programme to help impact the well-established link between work and health, and the importance of early intervention.
Local integration
Local integration is a key principle across all Working Well programmes. Each Local Authority has a designated local lead who will engage with the commissioned programmes and work with them to ensure the needs of the borough are met. This integration generally involves local Integration Boards – led by the local authority and attended by providers, and local services (health, skills, housing, drug, and alcohol etc.). The meetings are used to discuss local needs, challenges, barriers and opportunities with a view to linking existing local provision together to meet need and achieve greater outcomes for local residents.
Providers of commissioned programmes employ staff (integration co-ordinators) to engage with local stakeholders and work with them to implement a local integration plan. This will focus on the needs of the participants and, within the borough.
Local Authority representatives also have an opportunity to be involved at the bid review stage of the commissioning cycle, allowing them to have input into the commissioning process.
How to join-up with other partners and local services to establish an effective signposting and referral process?
Social prescribing
The NHS long-term plan set ambitious targets for the scaling up and rolling out of social prescribing. GM is ahead of the trajectory on social prescribing, with all ten localities having commissioned, social-prescribing programmes in place – the largest city region to be able to offer social prescribing across all local authority/CCG areas – and over 25,000 people supported through social prescribing in 2019/20
As part of the bid process for the Working Well Work and Health Programme, GMCA built in a requirement for a social prescription platform to be used across GM to help facilitate signposting and referrals across the wider support system. Traditionally, referral pathways have been difficult to implement and difficult to track.
The platform allows services to advertise their offer and manage the referrals that they receive, while allowing the provider to effectively refer participants to external support. The platform also allows for effective reporting and tracking of these referrals.
As the provider for WHP, JETS and Restart is the same, the platform and the services signed up to it can be shared across contracts. The platform enables GMCA to understand where our services meet client needs and if they do not, whether it is it due to poor service or gaps in commissioned provisions.
Integration with GPs
On Early Help the GP referral pathway is key. The HSCP helped to facilitate the initial discussions with local GP practices and helped to establish referral pathways into the programme.
A local provider was subcontracted to engage with the GP practices what were involved in Early Help. The provider had years of experience in engaging with GPs in GM and were able to set up “Fit Note Clinics”, and on-site method to support practices in making use of the WWEH programme.
JCP
To ensure that referral levels match the programme expectations, each Working Well programme has close on-the-ground relationships with all local JCP offices. JCP co-ordinators will present webinars, liaise with work coaches, and spend time in JCP offices to ensure referrals who will benefit most from Working Well Provision are able to start on programme. Any local issues, challenges or barriers can be quickly addressed by utilising the strong relationships in each borough between provider and JCP.
Adult Education Budgets (AEB) and Skills Support
The Work and Health Programme has no embedded skills offer, however GMCA has devolved responsibility for the AEB and so strong referral links have been created between this provision and local skills and training providers. Both WHP and JETS can refer directly into local skills provision, from basic skills to improve employability, to industry recognised qualifications. To date WHP has made over 25,000 referrals to AEB provision.
Successes so far:
Working Well: Work and Health Programme
- 20,000 programme starts
- Over 7,500 job starts
- More than 500,000 keyworker appointments attended
- Over 100,000 external referrals above and beyond
- Direct Delivery (work, health, skills, life interventions). That is on average five external interventions per person
- 70,000 referrals to the WHP (internal) Health Support Team.
Social value added:
- £100,000 charity fundraising
- Delivered 23 disability confident events to employers
- 900 days staff volunteering.
Liverpool City Region (LCR) covers a population of approximately 1.5 million and functions as a city region with a Combined Authority. The six council areas that make up the city region are Liverpool, Halton, Sefton, Wirral, Knowsley and St Helens.
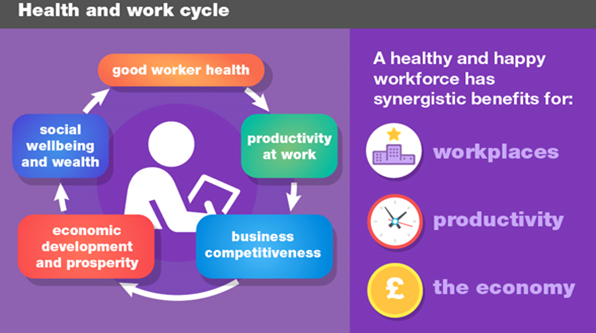
The Wealth and Wellbeing Programme in Liverpool City Region had its initial drive in the established link between work and health. Being in work is, generally, better for an individual’s health than not being in work and better still, if that work is shaped and structured in a way that enhances the health of employees.
From that starting point the programme developed the link between low productivity, a major concern of economic planners, and poor health and quantified the impact of poor health in terms of lower economic output. It was then a short step from knowing that the way the economy functions has a major impact on the health of the population to exploring just what it would mean if we started measuring economic success in terms of wellbeing outcomes.
The programme is now progressing to propose further investment in employee support programmes to help people suffering now from lack of employment owing to poor health and, to develop with people in communities what it would mean to plan the economy around wellbeing. Building on the National Health Science Alliance Wealth and Health report with further analysis by University of Liverpool, it was possible to quantify the impact of poor health on economic productivity in several ways.
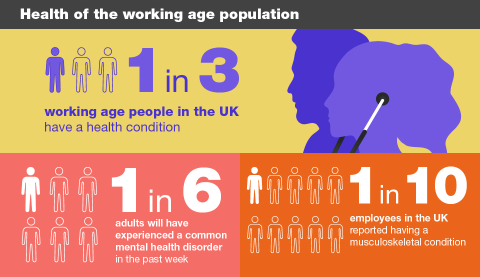
When looking at the gap in productivity between the economy of the LCR and the rest of the country, this analysis found that 33 per cent of the gap can be attributed to ill health. This equates to £3.2 billion in lost gross value added and that is about 10 per cent of the total economic output of the LCR economy on an annual basis. Further analysis by Public Health England made it clear that the major impact of health on the economy is though mental ill health and some way after that, through musculoskeletal problems.
A work and health profile was produced for the city region and for each of the six boroughs that make up the city region. Connecting across the system early in the programme the council leadership advised that the work should progress through engaging with communities and the bringing together of parts of the system that might not usually have much interaction. The emphasis was on a system leadership approach that invited views from as wide a range of perspectives as possible. This approach took its most tangible form in six workshops, one in each of the six boroughs, on a different aspect of the wealth and wellbeing programme. The intention was to place less emphasis on the presentation of good practice – although that is important at times – and to provoke discussion by posing questions. Workshop themes included links to the environmental agenda and asked whether it was more important to have a good job for everyone, or a good quality environment for everyone.
The workshops helped to engage people in discussion on work, health and the economy that would not otherwise have happened. A compelling narrative is important in any programme that is considering large scale change – to have a good understandable story at the core of the programme. It is crucial that, in this case, the story is built upon the views of people most affected by the current state of work and health.
A commission was undertaken to understand views on the social determinants of health and the role of local government. Views were secured from 21 people (out of 40) across the region who are experiencing the impact of ill health on employment. This has been written up in a report and presented in a video. It is the basis for development of a story about work, health and the economy in the LCR that will become a compelling narrative for change.
A review of the evidence-base on health and work showed good evidence for employee support programmes, particularly individual placement and support schemes for people with severe mental illness, but also others, as a sound investment to support people with health problems to engage with work again. Building on the good practice in the region in this area will be a feature of the programme as it moves into the next decade.
Much is being done through Fair Employment Charters, Healthy Workplace Charters and other activities to shape the workplace to be better for the health of employees. The Wealth and Wellbeing programme will bring a stronger health focus to this work in LCR and will take onboard the national reviews of the changing world of work to ensure that health for its own sake, and because we know that a healthy workforce is better for business, is prioritised.
Finally, the programme has tapped into the national and international interest in wellbeing economics. We engaged across the communities, health services, employers and councils of LCR and asked: what would it mean to have wellbeing at the core of economic planning for a city region; what would be different from the current focus of economic planning; what different priorities, actions and investment could follow if the main goal of economic planning was population wellbeing? By asking questions and inviting views from any quarter that is interested we believe that we stand a better chance of making a difference. We are establishing the belief that an economy that functions effectively for everyone is better for health and wellbeing and, a population with better health and wellbeing, is better for an effective and fair economy. Economic planning is therefore a legitimate interest of anyone interested in a healthier population.
‘Working in mind’ is an employability initiative targeting priority Jobcentre Plus clients – unemployed adults with mental ill health and older people with poor literacy skills.
Working with partners such as Redbridge Concern for Mental Health and other local mental health charities, the initiative combines traditional employability support, dyslexia screening, wellbeing coaches and access to social prescription provision, such as mindfulness training.
Around 50 per cent of participants progress into work, while others move into further learning.
Central London Forward’s £51 million devolved ‘Work and Health’ programme, ‘Central London Works’, aims to support 21,000 residents with health conditions and disabilities, and the long-term unemployed, into work.
Not only do CLF and Ingeus, the provider, work closely to assess referral numbers, job starts and the quality of jobs and support, they work with the boroughs to integrate borough-led and JCP provision including through ‘super centres’ in Hackney, Lambeth and Islington, which also helps to support employers’ recruitment needs.