Resetting the relationship between local and national government. Read our Local Government White Paper
The LGA and the Association of Directors of Public Health (ADPH) have jointly produced this briefing for Directors of Public Health about the public mental health and wellbeing issues arising from the COVID-19 outbreak.
Effective responses to the public mental health and wellbeing impact of COVID-19 will be essential to sustain the measures necessary to contain the virus and aid recovery. As the pandemic enters different phases, with a tiered approach replacing a second set of national restrictions, supporting the mental health and wellbeing of residents will continue to be a priority for councils.
The Local Government Association (LGA) and the Association of Directors of Public Health (ADPH) have jointly produced this briefing for Directors of Public about the public mental health and wellbeing issues arising from the COVID-19 outbreak. It reflects the core role of Directors of Public Health in response to a major incident as set out in the Government’s Guidance on the Director of Public Health (2020 revised), Health Protection in Local Government (2013), and summarised in an Association of Directors of Public Health major incidents checklist published in 2018. This note focuses on the public mental health impacts, but there is an important interface with councils’ statutory mental health responsibilities for children and adults when leading the pandemic response and recovery.
Public mental health and wellbeing impacts
While many people have acted in solidarity in response to COVID-19, and there are some positive benefits from this community spirit and response, early evidence shows that the pandemic is having a detrimental impact on the mental health of some people.
Public Health England (PHE) routinely compiles a COVID-19 surveillance report that updates and summarises findings from ongoing mental health and wellbeing surveys. The Centre for Mental Health recently estimated that up to 10 million people, including 1.5 million children and young people under 18, may need mental health support in the aftermath of the pandemic.
The many psychological impacts of the epidemic on the population will have a detrimental effect on the short, medium and long-term mental health of some residents. In turn, this may reduce people’s resilience and their ability to cope. Longer-term impacts in terms of trauma, grief and distress may exacerbate the burden of mental ill-health in the community long after recovery. The mental health impacts will not be experienced equally: people with existing mental health difficulties and risk factors for poor mental health are likely to be affected disproportionately.
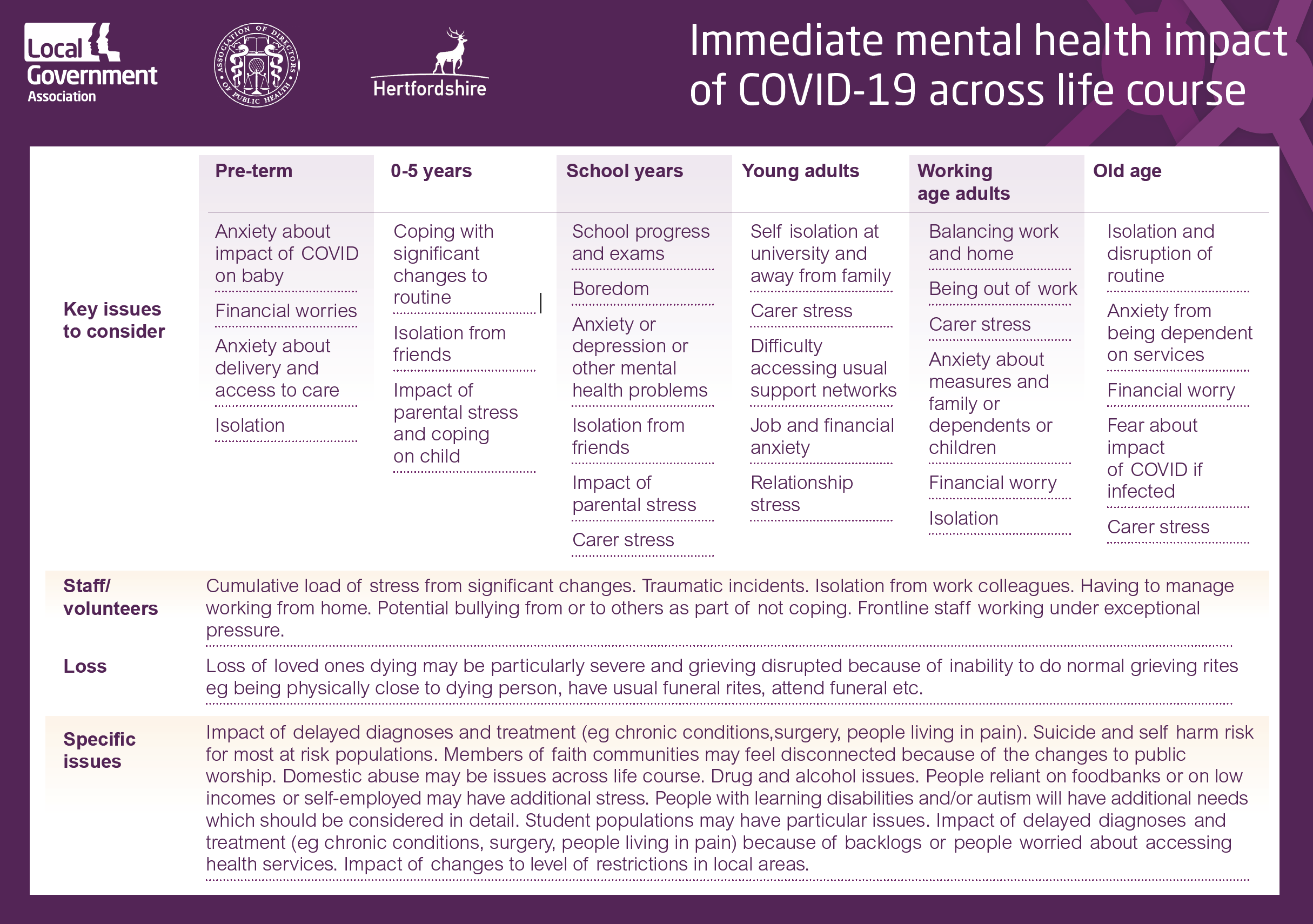
The behaviours and environments needed to curtail the spread of COVID-19 are known risk factors for mental health difficulties. The diagram below shows potential mental health impacts of COVID-19 across the life course. There will be additional impacts for people with a learning disability and/or autism which will need careful consideration. Students and frontline staff are likely to have additional impacts too.
Some people will experience trauma – that is harmful experiences or life-threatening events that can have lasting impacts on mental, physical, emotional and/ or social well-bring. It is a normal part of a human response to major emergencies and may not require specific medical support unless Post Traumatic Stress Disorder (PTSD) is diagnosed. But there are a range of harmful impacts which may result, including anxiety, depression, inability to cope, grief and loss from bereavement, domestic abuse and crowd behaviour which creates social norms which reinforce harmful behaviours (for example, panic buying making those vulnerable less able to cope).
There may be additional stress for people who must make major lifestyle changes, such as people living in parts of the country affected by stricter restrictions, people who are self- isolating, people who have had procedures or medical treatment postponed (this could include children or young people waiting for CAMHs assessment) additional advice for the medically extremely vulnerable, especially when people do not have access to support networks and as a result of any re-introduction of formal shielding arrangements.
These impacts could be short-term (for the duration of the epidemic), medium-term (2 year) or long-term. They can be experienced by all sections and all ages of society. Consequences could include increased demand on local government and the NHS, increased suicide, suicide attempts and self-harm, increased cost to public services and increased workplace sickness absence due to stress.
|
Short-term impacts |
|
|
Medium- term impacts |
|
|
Long-term impacts |
for children and young people:
|
Key principles of local responses
Directors of Public Health will as part of responding to COVID-19 prioritise locally the work they are undertaking. Public mental health in all aspects, including but not limited to suicide risk, should be considered as part of understanding and responding to the burden of ill-health and promoting wellness.
Key principles underpinning local responses include:
- Whole-system approach – no single agency can be left to address this by themselves; it needs input from all sectors including voluntary, statutory, employer and faith - as well as local neighbourhood action.
- Life-course and whole family/household approach – an evidence-based understanding of local need and interventions that target the whole population (including children and young people), populations at higher risk and people who need additional support (linking to wider work to support people in vulnerable circumstances). This includes recognising that mental ill-health affects the whole family or household, beyond any individual who receives support, and links to children’s and adult’s statutory mental health services.
- Build on existing arrangements – for example, mental health programmes for young people, multi-agency suicide prevention partnerships and bereavement networks. Also building on existing local and national resources that promote wellbeing and healthy ageing.
- Tackling inequalities – have mental equality in mind when responding to the outbreak and planning for recovery. The determinants of mental health interact with inequalities including communities of geography, ethnicity and gender in ways that put some people at a far higher risk of poor mental health than others. COVID-19 has potential to exacerbate these inequalities.
- Apply learning from the first wave – build on local intelligence about residents supported during the first wave who might need further support, as well as identifying residents who have become more vulnerable due to the direct and indirect consequences of the pandemic. Importance of supporting people who are lonely, especially during Winter months. Workforce resilience.
- Good communication - both to professionals and to the public. Particularly aimed at reassurance and building resilience, including the role of councillors. Ensure strong system links – that organisations are aware of what support and advice is available from councils and other local organisations and nationally from Government and sector representative bodies (ADPH, LGA). Highlight positive examples of communities coming together and supporting each other.
What councils are doing
Councils are working hard with the NHS, schools, employers and other local partners, especially the voluntary and community sector, to support the mental health and wellbeing of their residents, including children and young people, and will continue to do so as we enter different phases of the pandemic.
Actions across the mental health spectrum include continuing to meet statutory responsibilities for adults and children’s mental health needs, supporting the mental wellbeing of frontline staff, bereavement support, suicide prevention, helping residents to stay connected, supporting mental wellbeing in schools, and supporting people who might need additional help such as unpaid carers and new parents. Councils also promote mental wellbeing through, for example, safe access to parks, youth services, children’s centres, open spaces, encouraging physical activity and expanding public libraries’ online offer.
There is a COVID-19 public mental health Community of Practice on the Knowledge Hub for public health practitioners and organisations with an interest in addressing the mental health impacts of COVID-19 to share what councils are doing, documents and connect with each other. In August 2020 the LGA and Centre for Mental Health published Our Place which examined how nine councils are promoting good mental health and preventing poor mental health in communities, including early learning from COVID-19.
Further information
LGA has a range of information on coronavirus for councils on their website and resources to support workforce health, resilience and wellness during COVID-19. There is also a wellbeing guide for staff working in schools and trusts.
PHE has issued Guidance for the public on the mental health and wellbeing aspects of coronavirus (COVID-19) and Guidance for parents and carers on supporting children and young people’s mental health and wellbeing during the coronavirus (COVID-19) outbreak
PHE has also updated the Every Mind Matters platform with specific advice on maintaining good mental wellbeing during the outbreak, including looking after a child’s mental health and self-care for young people.
Real World Public Mental Health podcast, hosted by the Behavioral Science and Public Health Network (BSPHN), looks at how evidence is being used in the real world to prevent and promote better mental health for all. It is part of a public mental health collaboration between BSPHN, PHE, ADPH, LGA, Centre for Mental Health, Mental Health Foundation and NIHR – School for Public Health Research. The podcast series follows the webinar Prevention and Promotion for Better Mental Health in Local Systems, hosted by PHE in November 2020 on behalf of the collaboration, which can be viewed on the COVID-19 public mental health community of practice.
DHSC Staying mentally well: winter plan 2020 to 2021
Revised government guidance on shielding and protecting extremely vulnerable people from COVID-19.
Young Minds has produced tips, advice and information on where to get help during the COVID outbreak.
Mind resources on Coronavirus and your mental health
WHO advice ‘mental health considerations during COVID-19 outbreak’
Centre for Mental Health COVID-19 and the nation's mental health: forecasting needs and risks in the UK
The Royal College of Psychiatrists has prepared guidance to help their members provide the best mental health services possible during the Covid-19
The Institute of Health Visiting has published COVID-19 Professional advice for Family Perinatal Mental Health