With their emphasis on accessibility, wellbeing and community, arts, sport, parks, leisure services and museums are all well-placed to deliver on a range of policy objectives and contribute to local recovery strategies.
Prescribing to arts and culture
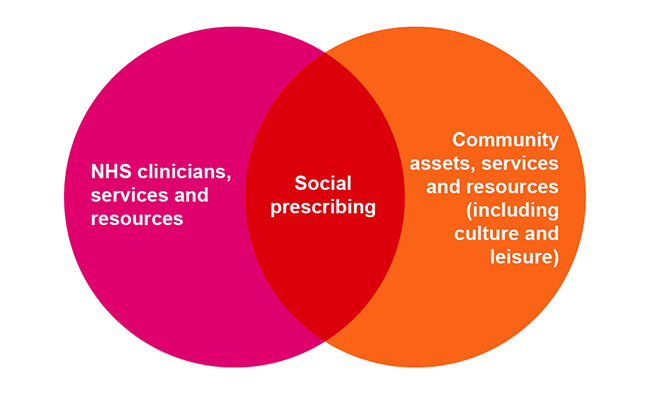
The arts can have a powerful impact on people with long-term health conditions. For example, music therapy reduces agitation and need for medication in 67 per cent of people with dementia. Many councils are already delivering social prescribing programmes such as arts-on-prescription and museums-on-prescription (sometimes known as referral programmes such as arts-on-referral). This involves people experiencing psychological or physical distress being referred (or referring themselves) to engage with the arts in the community including galleries, museums and libraries.
Arts on Prescription Gloucestershire has shown a 37 per cent drop in GP consultation rates and a 27 per cent reduction in hospital admissions. This represents a saving of £216 per patient The APPG on Arts, Health and Wellbeing Inquiry cites a social return on investment of between £4 and £11 for every £1 invested in arts on prescription.
Wonder Women is an empowering project set up by Peterborough Council for Voluntary Services’ Women’s Forum. It included a series of creative art workshops hosted by arts organisation Metal with intuitive artist Sa’adiah Khan. The workshops were well attended, providing attendees the opportunity to meet each other and engage in conversation, while experimenting with various forms of art making. The women enjoyed exploring messy art, being playful, learning new skills and having fun with various materials. Being creative while spending time connecting to others in a safe and friendly environment proved a real boost to their mental health and wellbeing. Participants enjoyed “making art without pressure” and found it a good outlet to express themselves, in a safe environment. “These sessions have given me the opportunity to have open and safe conversations with other woman, while being creative and making."
Other examples of arts and culture social prescribing programmes include:
- Dementia cafes supported by the Alzheimer’s Society, these cafes have sprung up around the country – usually in museums, art spaces or libraries, offering people with dementia, and their carers, a safe, friendly place to relax and socialise and enjoy the sights on offer at the cultural venue.
- Knit and natter groups bring people together socially in a group where they are occupied and conversation can flow easily.
- Using archaeology to aid the recovery of military veterans: the Ministry of Defence launched Operation Nightingale in 2011 with the aim of involving wounded, injured, and sick military personnel and veterans in archaeological investigations as part of their recovery. One of the participating archaeological sites was Buster Ancient Farm in Hampshire, 26 volunteer veterans worked with archaeologists to build a traditional Bronze age round house. The build had a significant impact on the volunteers who took part.
“Working through each stage of the project has been brilliant and I still find it hard to believe how much my life has turned around because of it. Not just feeling myself again, gaining more independence and confidence, the comradery but what else the project has led onto.”
— John William Bennett, Royal Navy Veteran, 2021 Archaeology Undergraduate
Prescribing to libraries
Councils have a statutory duty to provide a comprehensive service, and to encourage both children and adults to make full use of the library service and to lend books and other printed materials free of charge to people living, studying, or working in the area. They are non-judgemental spaces that everyone in the community has access to, giving them a unique role in supporting people with health conditions, connecting and supporting communities. This is exemplified through the following examples:
- Reading well books on prescription (or bibliotherapy scheme) makes self-help books readily available to people to encourage greater understanding of their health condition and to learn how to better manage mental health issues such as anxiety and depression. Most libraries have a well zone where such books can be found.
- Reading groups encourage people to share their thoughts about particular books or simply to sit quietly and listen to a book being read – story time for adults if you like. While groups for children encourage them to see the library as a part of their community, offering as much or as little about books as they want but providing a social space for their parents and carers who may often find themselves socially isolated at home with young children.
Prescribing to sport
The link between exercise and health is clear. Sport can also offer other benefits through social prescribing, such as a sense of enjoyment and fulfilment, and helping people connect to others and their community. Exercise on referral is one of the earliest forms of social prescribing and is usually a programme where people with long-term health conditions such as diabetes, high blood pressure, or heart disease increase their physical activity levels by regularly using local leisure centres through GP and other referrals. Like with culture and arts, sports related social prescribing needs to be imaginative and varied, tapping into activities that support people who are experiencing a range of physical and mental health conditions and wider issues like loneliness or social isolation.
East Riding of Yorkshire Council’s exercise on referral scheme and the Live Well scheme continue to flourish with GPs able to refer directly via a secure e-referral system. The referral is picked up by the Central Team the day the referral is made, and they will attempt to contact the patient within 48 hours. While the exercise-on-referral is a set period of 10 weeks – Live Well can last up to a year. Over the past year about 1700 exercise on referrals have been made and 258 Adult Live Well referrals and 230 Young Live Well referrals.
Other examples include:
Singing can be its own exercise and can be beneficial to those who may, for example, have Chronic Obstructive Pulmonary Disease (COPD).
Royal Brompton & Harefield NHS Foundation treats patients with complex diseases and conditions. In 2002
rb&hArts was set up to run innovative arts programmes for patients. In response to the Covid-19 pandemic, rb&hArts successfully piloted online Singing for Breathing sessions for 117 participants specifically aimed at people living with chronic or life-limiting respiratory conditions and were required to shield. The singing sessions provided physical exercise which supported lung function and vital space with time for a chat. The programme boosted positive mental health and created peer support networks.
- Swimming is a low impact exercise that can be done at an individual’s own pace and enhances mood and fitness.
Swim England ran a three year project to provide swimming for people with dementia and their carers. The project provided guidance to pools on signage and safety for people with dementia to ensure a safe space for them to enjoy the water. Health outcomes included enjoying the benefits of exercise, increased confidence in the water and an opportunity to work off some of the frustrations that both people with dementia and their carers can experience. The project was supported by DHSC funding and required the development of strong partnerships across a diverse range of public and private organisations, charitable trusts, council officers, care providers and community nurses to deliver the programme. Two pilot sites were introduced in Manchester and Durham in 2015. A year later this expanded to five including some of the London boroughs and by year three, 2017, a total of 48 pool operators were involved.
Green social prescribing
Green social prescribing links individuals to nature-based interventions and activities, such as local walking for health schemes, community gardening and food-growing projects. The pandemic highlighted the importance of being outdoors to people’s mental and physical health as well as the inequality of access to private gardens and green spaces. Some innovative examples include:
- Gardening can provide a ‘dose of wellbeing’ as demonstrated by the Eden project’s social prescribing project “Nature’s Way”. The activity and creativity of working with plants and meeting others is helping to boost physical and mental health, reduce isolation and instil a sense of purpose.
- Partnerships and referral pathways between local mental health services and social prescribing can help to reduce demand on services and provide alternatives to traditional therapies.
The
‘Connecting in Nature’ programme provided local Brighton and Hove residents the opportunity to connect with themselves, each other and nature as a way of supporting their mental health and well-being. While the project was promoted by the local social prescribing service, most participant referrals came through the partnership with MIND. The impact of the project was overwhelmingly positive with 100 per cent of attendees noticing a positive impact on their wellbeing from attending these sessions “Time in nature does me good, but I struggle with the motivation to do it on my own...the group gave me a much needed boost each week” Attendee, Connecting in Nature group autumn series.
Points to consider:
- Is your council’s culture and/ or sports and parks services maximising their contribution to social prescribing? How could this be developed? Can you broker introductions to health services or link workers?
- How can you support sports, arts and cultural organisations in your area to get involved in social prescribing or expand?
- What are the referral pathways into social prescribing activities? Could these be developed further or does it need to be streamlined? Is it a clear route and easy to navigate by service users and link workers?
- What are the key community spaces in your area? For example leisure centres or libraries, and can these be used to signpost people to a wider range of services and social prescribing opportunities?
- Who are the community leaders in your area? How can you work together to reach underserved groups?
Measuring impact
There is an emerging body of evidence that social prescribing can contribute to a range of local and national priorities, as outlined in the making the case section.
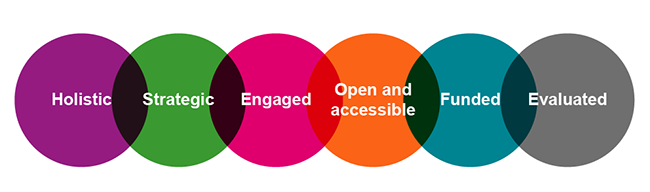
Measuring the impact of your social prescribing initiatives is a powerful tool for building the case for investment, as well as helping you to understanding the impacts you are having. There is not a ‘one size fits all’ approach to evaluating the impact of social prescribing but it is important to have consistency in the data that’s collated so that effectiveness can be assessed.
If possible, try to encourage local partners to adopt the same or similar evaluation frameworks so you can compare results. You may also want to think about how you can build the capacity of smaller organisations to measure impact, for example by sharing knowledge and resources.
For a comprehensive introduction to evaluation and the various tools available, the ‘Look I’m Priceless’ guide is helpful. Although developed in 2016, the Public Health England framework for evaluating the impact of arts programmes on health wellbeing is still relevant as is the Creative and Credible guide (2015). The New Economics Foundation’s guide for measuring impact on wellbeing is aimed specifically at voluntary and community organisations.
There is also more targeted guidance available, such as the ‘What works well for wellbeing’ guide to measuring impact on loneliness. UCL have developed a tool for museums to evaluate their impact on wellbeing and Sport England have created a comprehensive evaluation guide for sport and physical activity initiatives.
The NHS has developed an outcomes framework aimed at measuring three key aspects of social prescribing. All link workers employed by the NHS will be working with this outcomes framework, and it is therefore important to bear this in mind when designing local social prescribing programmes and evaluation processes. Make sure you are in regular dialogue with link workers and talk to them about how you can work together to support evaluation and share results for mutual benefit.
Supporting social prescribing in your area
We hope this guide has helped you to understand social prescribing, the role of arts and culture in its delivery, and that the case studies have inspired you to think creatively about the wealth of ways through which you can improve your residents’ health and wellbeing.
There are a number of common themes found across the case studies which may be helpful to bear in mind as you go forth and develop your local social prescribing offer.
- Local leadership is key to building across organisational boundaries – include PCNs, ICSs, ICBs, ICPs, voluntary and community sectors, social care and public health, GPs, link workers and local patient and carer groups.
- Consider your approaches to commissioning, is it accessible to community organisations already delivering social prescribing?
- Take a holistic approach - if you have not already done so, bring together organisations that include the arts, cultural and leisure sectors, to identify ways that all can contribute to improved health and wellbeing for residents
- The buy-in of senior leaders and decision makers is key to developing understanding, investment and support for the frontline.
- Make social prescribing a key focus for health and wellbeing boards and ICSs.
- Identify strategic and commissioning opportunities to advocate for inclusion of using arts and cultural and leisure providers to improve health.
- Nurture and invest in capacity especially of small organisations, support training and development initiatives for libraries, culture and leisure staff.
- Take contracting approaches proportionate to the value and complexity of the services being provided to avoid excluding small community groups.
- Small community groups need support, development and training rather than over complicated processes and regulation. Maintain close partnerships so that problems can be aired quickly and solutions reached.
- Consider your referral pathways, are they fit for purpose, are they maximising the opportunities or do they need to be simplified?
- Share and promote examples of social prescribing already in action.
- Offer in-kind as well as financial support. For example, offering a venue for activity sessions or office space at a reduced rate, or providing an IT platform to advertise community events. This can particularly help to build the capacity of small voluntary and community sector organisations and may unlock greater opportunities.
It is crucial to work in partnership with local health organisations and the VCSE to understand your current local offer for social prescribing. Then, you can identify key assets and gaps, and develop a strategy to sustain and grow the offer. Finally, be creative about grant funding opportunities from organisations like Arts Council England, Sport England and the Big Lottery Fund which might align with your objectives. The focus of these may be on culture (for example) rather than health but making the connection with wellbeing can help to encourage new and diverse audiences through the door while improving physical and mental wellbeing and sharing the joy of local collections, parks or leisure activities.