This case study describes Dorset’s progress developing integrated care arrangements. It is part of an evidence review commissioned from the Institute of Public Care.
Strong and collaborative leadership is the cornerstone of Dorset’s ability to deliver its health and wellbeing agenda through integrated services. After a bumpy start with a lack of understanding of each other’s roles and responsibilities, leaders of the Council (members and officers) and the CCG started to meet informally and get to know each other over tea and cake. Relationships improved and despite their different cultures, systems and processes, leaders recognised the need to work together. Focusing on the needs of their population, they rapidly established a joint strategy and work plans to tackle local challenges. These include providing care in rural areas, a CCG footprint that includes two Better Care Fund plans and a significant lack of affordable/suitable housing that impacts negatively on staff recruitment and retention as well as the growing elderly population.
New approaches include the ‘Dorset Care’ contracting framework, initially focused on home and community care, which also enables rapid response to arising pressures within the NHS and is proving to be a flexible resource. Another innovative development has been the establishment of ‘mini-Health and Wellbeing Boards’ based on GP localities which bring together a wide range of relevant local partners from health, social care, housing and the voluntary sector to establish place based plans and responses at a micro level.
With a focus on people rather than structures, the join-up between health and social care is aided by joint public engagement forums, joint workshops for staff working on different strands of the work programme and the appointment of a joint Director of Public Health with the CCG which is key to enabling a focus on prevention and wellbeing for the local population.
Introduction
The Dorset Sustainability and Transformation Partnership (STP) plan commits partners from across the health and social care sector to adopt a whole system approach to improving health and care outcomes:
“We will work with people, communities and other organisations to improve and maintain their wellbeing, to live as independently as possible recognising that some individuals may need more support than others.”
The contribution towards this system wide plan from Dorset County Council adult social care has been focused on three key outcomes:
- delivering good health and care – affordable, flexible and accessible
- promoting independence – helping people to help themselves
- enhancing wellbeing for local communities.
This joined up approach to providing care for the population has enabled Dorset to be included as one of the eight ‘first wave’ local systems to become an Integrated Care System. Building on formal governance structures and pooling of funding arrangements such as the Better Care Fund (BCF), Dorset is working on transformational activities such as progressing integration across all age groups and across commissioning and delivery. For example, health, social care and district councils have joined up their provision of community equipment, minor and major adaptations and assistive technology to promote personal independence. Where it makes sense, they are also exploring pooled arrangements with colleagues in neighbouring Bournemouth and Poole. A single pan Dorset public health function supports the Health and Wellbeing Boards and the STP.
Governance, leadership and commitment
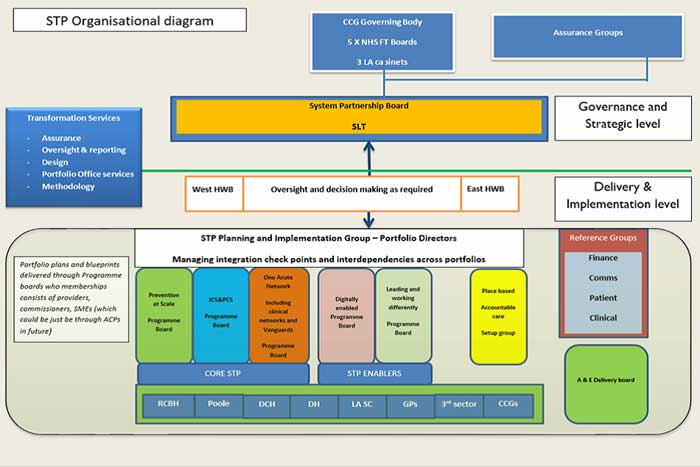
The governance diagram below has been created to show the interactions between key boards. The Systems Leadership Team includes representation from elected members of the relevant portfolio boards to provide strategic direction. They are supported by the Health and Wellbeing Boards which have the shadow East and West Integrated Health Care Partnership Boards aligned to them. Within this governance structure, there is an on-going focus on data to influence and shape future modelling and spend.
Whilst the governance arrangements allow for formal decision making, and a shared understanding of roles and responsibilities across the system, partners agree that it is effective relationship building, both formally and informally, that provides the glue to holding it all together.
Also of note, the importance of culture has been recognised as a key enabler or potential barrier to the success of transformation plans within the area. Plans are in place across the County Council and CCG to tackle and address culture issues to better understand other’s roles, reactions, resource limitations, team structures and capacity to facilitate the transformation in service delivery that will lead to improved health and care outcomes.
Delivering integrated care
As previously mentioned, one of the key drivers for delivering integration is the Better Care Fund, underpinned by several joint funding arrangements between the local authorities and the CCG. Across the BCF and transformation programme, there are a number of key initiatives and projects focused on integration:
- Support for carers
- Integrated health and social care pathways
- Maintaining independence
- High impact changes
- Moving on from hospital living
- Sustainable care markets
Two examples of key work streams are as follows. Firstly, Dorset’s Adult Social Care Asset Strategy 2018-2028 sets out the need for different models of housing with care, including relocatable housing, to help meet demand and relieve pressure on hospital delays. To deliver this, a programme of change ‘Building Better Lives’ is in place which is working closely with the STP Estates workstream to ensure that a joined-up approach to the reduction of community hospitals and development of primary and community care hubs is in place and these are also connected to local neighbourhood plans that set out local housing development plans. Six locality blueprints have been developed based on population projections and existing demand information. This includes a mixture of accommodation with care, care homes and relocatable modular housing for adults with learning disabilities.
Secondly, strong leadership of the local care market and integrating commissioning, quality and brokerage is being exercised through a joined up CCG and Dorset County Council approach to proactive care market management. A contract framework has been put in place called ‘Dorset Care’, initially focusing on home and community services for older people, which commenced in December 2017 and is now extending into learning disability and mental health services.
The Dorset Care Framework provides a platform for joined-up dialogue with the market and creating rapid solutions for arising pressures. For example, the
Framework was used to create a rapid response to winter pressures, funded by the local hospital to improve the timely discharge of patients.
Dorset also recognise that the care market and their contracting approach needs to reflect the high proportion of older people within the area who will be responsible for funding their own care and the impact this has on designing the right housing and interventions to achieve prevention at scale for this population. Public participation has been key to the development of Dorset’s plans with extensive consultation having taken place across the county.
Next steps
The System Partnership Board is in discussions about the use of ‘control totals’ across the whole health and social care system within the area, where budgets and assets will be pooled to achieve the outcomes within their shared plans.
The Partnership Board is also looking to add the Transport Board to their governance structure in the recognition of the key role that transport plays in maintaining the health and wellbeing of the local population and to ensure transport resources are being most effectively deployed to achieve this.
Download Integrating health and social care: Dorset case study