Introduction
Helping people to achieve and maintain a healthier weight is everyone’s business. As an elected member your decisions can have a significant and positive impact on health improvement in your local area. We have known for decades that living with obesity reduces life expectancy and increases the risk of developing chronic diseases. Living with obesity can also affect people’s mental health and their social and emotional wellbeing. It has become more apparent than ever that excess weight is a serious matter, given the over representation of people living with obesity, having contracted COVID-19, in intensive care units (ICU) worldwide. All of this can affect people’s life opportunities and has a direct impact on the community.
The necessary measures to suppress COVID-19 may have increased the risk of weight gain, whilst also making it harder to access weight management services. We have seen changes in the patterns of food purchases and physical activity that may be associated with increased calorie intake, increased sedentary time and excess weight gain. There have also been changes in economic and psychosocial factors – such as rates of unemployment and mental illness - that have also been linked to excess weight gain.
Since the majority of adults in England are living with overweight or obesity, and a substantial number of children are on the same trajectory, tackling obesity remains one of the greatest health challenges this country faces. In a reflection of our shared commitment with government, local authorities have been offered additional funding for the expansion of weight management services, as part of a whole systems approach to tackling obesity. Given the socio-economic disparity in healthy life expectancy in England, tackling obesity is fundamental to, and at the heart of, the levelling-up agenda.
Key messages:
- Almost two-thirds (63 per cent) of adults, and one in three children in England are living with overweight or obesity.
- Behavioural weight management services for adults living with overweight or obesity are multi-component programmes that aim to reduce a person’s energy intake, improve their dietary health and help them to be more physically active by changing their behaviour.
- There is good evidence that behavioural weight management services can help adults to lose weight in the short term.
- Providing access to weight management services is a key part of a whole systems approach to obesity and promoting healthier weight, alongside other actions at a national and local level.
- Societal changes associated with the necessary measures required to suppress COVID-19 may have increased the risk of weight gain, whilst also making it harder to access weight management services.
- In a reflection of our shared commitment to tackling obesity, the government has invested over £30 million into local authority commissioned adult behavioural weight management services. For children and families, £4.3 million has been invested to expand behavioural weight management services and deliver extended brief interventions.
- Learning from this one-year programme of funding will help to make the case for more sustained funding for weight management services in future years.
- Local authorities are encouraged to provide equitable access to population groups most in need, including men, people living with obesity from deprived areas and people from Black, Asian and Minority Ethnic groups, and also to enable inclusive services for people with protected characteristics.
- As elected members, your understanding of local communities will enable you to work effectively with officers to ensure that the new funding is applied to meet the needs of local people.
The scale of the issue
Obesity is a complex relapsing condition with multiple causes and significant implications for health and beyond. It has health implications at every stage across the life course, from pregnancy through to childhood and adulthood. Living with obesity increases the risk of developing chronic diseases, including type 2 diabetes, heart disease, many cancers, liver and respiratory disease. There is also now consistent evidence that people with COVID-19 who are living with obesity are at an increased risk of severe complications of COVID-19 and death.
Almost two-thirds (63 per cent) of adults in England are living with overweight or obesity, and one in three children leave primary school living with overweight or obesity, with children from more deprived areas twice as likely to be living with excess weight compared to children from less deprived areas.
What are weight management services?
Behavioural, or lifestyle, weight management services, for adults living with overweight or obesity, are multi-component programmes that aim to reduce a person’s energy intake, improve their dietary health and help them to be more physically active by changing their behaviour. These services are usually commissioned by local authorities and/or the NHS and typically last for at least 12 weeks.
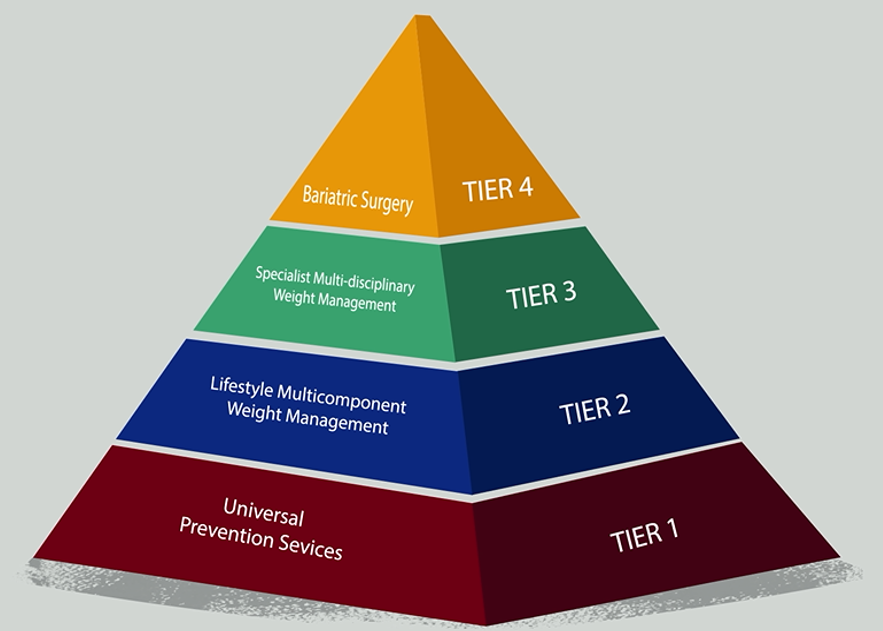
There are different levels of weight management services. Behavioural services, referred to locally as tier 2, form one part of a comprehensive approach to preventing and treating obesity.
Public Health England’s (PHE) guidance on commissioning and delivering tier 2 adult weight management services can help local areas in setting up effective services.
Why invest in weight management services?
For people living with obesity, even modest weight loss has been shown to bring long-term health benefits. Weight loss of 5 per cent reduces a person’s risk of developing diabetes, lowering blood pressure and cholesterol. It is also possible that the benefits of weight loss could mitigate COVID-19 severity.
There is good evidence that behavioural weight management services can help adults to lose weight in the short term.
Given the wide-ranging implications of living with obesity on health and beyond, it is clear that investing in weight management services is beneficial to individuals and the wider community.
How does investment into weight management services support a whole systems approach?
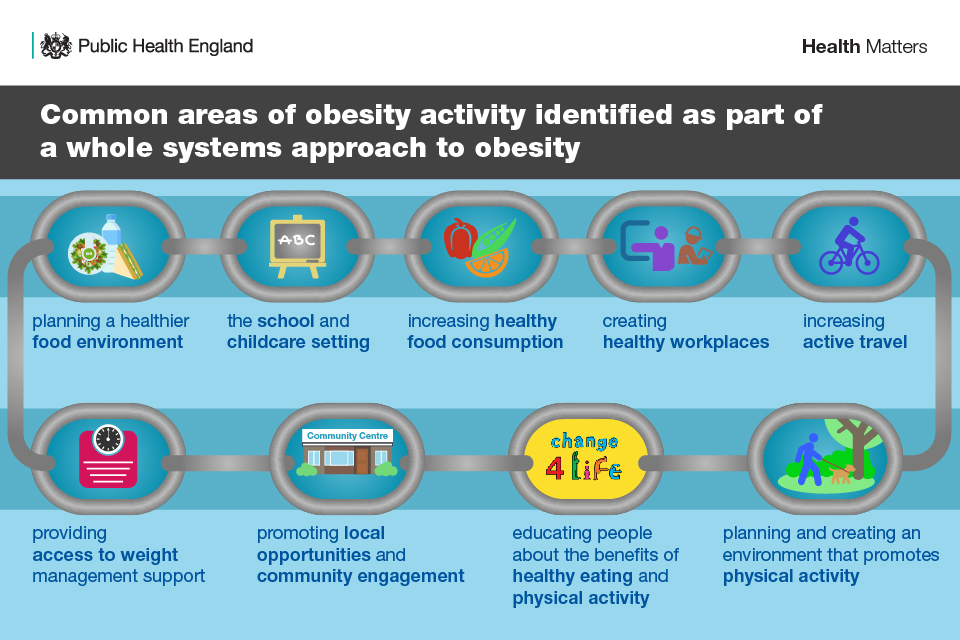
Improving and increasing access to weight management services, for the large numbers of people who could benefit from them, is a key part of a whole systems approach to tackling obesity.
The integration of these services alongside other actions at a national and local level strengthens and increases the effectiveness of the system, in supporting people living with overweight or obesity to achieve and maintain a healthier weight.
At a local level, PHE, in partnership with the Local Government Association (LGA), Association for Directors of Public Health (ADPH) and local authorities, has co-developed and published guidance to support local areas in implementing a whole systems approach to obesity and promoting a healthier weight.
At a national level, there is a wide programme of work underway to address obesity and help adults and children to live healthier lives. This includes commitments to further restrict the advertising and promotion of less healthy food, as well as improving front of pack labelling on pre-packed foods, introducing calorie labelling within out-of-home businesses, including restaurants, cafes and takeaways, and calorie labelling of alcoholic drinks.
These are all policy actions designed to empower and support everyone to have access to healthier options and access support to achieve and maintain a healthier weight, through bringing about change across the system.
Increasing equitable access to weight management services
Insight gained from local authorities has shown that the pandemic has reduced access to weight management support for children, young people and adults, and these changes are felt by officers to have increased inequalities.
Some groups of people are likely to benefit from different ways of engaging them in services, and from services which are tailored to their needs and how they live their lives. Such groups include men, people living with obesity from deprived areas, people from Black, Asian and Minority Ethnic groups, and people who are also living with physical and/or learning disabilities.
Providing equitable access to weight management services to population groups most in need is an essential part of supporting communities disproportionately affected by the drivers of obesity and addressing inequalities. Evidence based services must be adapted to make them culturally competent and relevant to the needs of population groups.
Elected Members as systems leaders
As elected members you are pivotally placed to champion this investment into healthier weight in your local area, engaging the local community and collaborating with officers.
Your understanding of local communities will enable you to work effectively with officers to ensure that the new funding is applied to meet the needs of local people. This will be vital in achieving the ambition for services to prioritise helping those who need the most support to achieve a healthier lifestyle, including men, people living with obesity from deprived areas, Black, Asian and Minority Ethnic groups, and who are also living with physical and/or learning disabilities.
The provision of active involvement and ongoing and visible support will send a clear signal that tackling obesity, as a part of a whole systems approach, is a priority for the local area. The commitment and support of members will also help to ensure that sufficient time and resource will be available to maintain momentum.
Questions to consider
The following questions apply to lead members, but all members may wish to consider them:
- Is the council providing weight management services to support people already living with obesity, alongside preventative actions?
- What measures are in place to support underserved/at risk communities in accessing weight management services?
- How does a whole systems approach to tackling obesity and promoting a healthier weight, including weight management services, feature in the council’s overview and scrutiny process?
- Has the council used data on its services previously and how does data that is routinely collated and provided feature in scrutiny committee?
- How is the council monitoring and evaluating progress on actions that are in place to tackle obesity and related drivers, including weight management services?
- Is the council working with the NHS to align weight management services?
- Does the council have a shared vision, narrative and communications strategy in place to communicate publicly why tackling obesity is important and the approach the council is taking to address it?
- Are all council departments contributing to tackling obesity through their relevant functions? Do other departments clearly understand how tackling obesity benefits their own agendas?